
 |
| |
|
|
|
#1
| ||||||
| ||||||
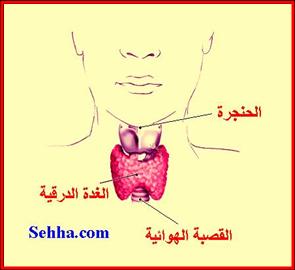
| بسم الله الرحمن الرحيمشخباركم وشعلومكم بدخل في الوضوع على طول من دون لف ودوراناخوانيواخواتيممكن تساعدوني في بحثي عن الغدة الدرقية ((thyroid)) باللغةالانجليزيةاريد معلومات وامراض الغدة الدرقية وكل شي يخص الغدة الدرقيةوبكون شاكرة لكم المصدر: منتديات مدينة الاحلام shu],kd [.h;l hggi odvh |
| | رقم المشاركة : [2] | |||
| The thyroid gland is a butterfly-shaped organ and is composed of two cone-like lobes or wings - lobus dexter (right lobe) and lobus sinister (left lobe) - connected with the isthmus The organ is situated on the anterior side of the neck, and is lying against and around the larynx and trachea, reaching posteriorly the oesophagus and carotid sheath. It is starting cranially at the oblique line on the thyroid cartilage (just below the laryngeal prominence or Adam's apple), and extending inferiorly to the fourth to sixth tracheal ring[citation needed]. It is inappropriate to demarcate the gland's upper and lower border with vertebral levels as it moves position in relation to these during swallowing. The thyroid gland is covered by fibrous sheath, the capsula glandulae thyroidea, composed of an internal and external layer. The external layer is anteriorly continuous with the lamina pretrachealis fasciae cervicalis and posteriorolaterally continuous with the carotid sheath. The gland is covered anteriorly with infrahyoid muscles and laterally with the sternocleidomastoid muscle. Posteriorly, the gland is fixed to the cricoid and tracheal cartilage and cricopharyngeus muscle by a thickening of the fascia to form the posterior suspensory ligament of Berry[1][2]. In variable extent, Zuckerkandl's tubercle, a pyramidal extension of the thyroid lobe, is present at the most posterior side of the lobe[3][4]. In this region the recurrent laryngeal nerve and the inferior thyroid artery pass next to or in the ligament and tubercle. Between the two layers of the capsule and on the posterior side of the lobes there are on each side two parathyroid glands. The thyroid isthmus is variable in presence and size, and can encompass a cranially extending pyramid lobe (lobus pyramidalis or processus pyramidalis), remnant of the thyroglossal duct. The thyroid is one of the larger endocrine glands, weighing 2-3 grams in neonates and 18-60 grams in adults, and is increased in pregnancy[citation needed]. The thyroid is supplied with arterial blood from the superior thyroid artery, a branch of the external carotid artery, and the inferior thyroid artery, a branch of the thyrocervical trunk, and sometimes by the thyroid ima artery, branching directly from the aortic arch. The venous blood is drained via superior thyroid veins, draining in the internal jugular vein, and via inferior thyroid veins, draining via the plexus thyroideus impar in the left brachiocephalic vein. Lymphatic drainage passes frequently the lateral deep cervical lymph nodes and the pre- and parathracheal lymph nodes. The gland is supplied by sympathetic nerve input from the superior cervical ganglion and the cervicothoracic ganglion of the sympathetic trunk[citation needed], and by parasympathetic nerve input from the superior laryngeal nerve and the recurrent laryngeal nerve. This section does not cite any references or sources. (January 2008) Please improve this section by adding citations to reliable sources. Unverifiable material may be challenged and removed. In the fetus, at 3-4 weeks of gestation, the thyroid gland appears as an epithelial proliferation in the floor of the pharynx at the base of the tongue between the tuberculum impar and the copula linguae at a point latter indicated by the foramen cecum. Subsequently the thyroid descends in front of the pharyngeal gut as a bilobed diverticulum through the thyroglossal duct. Over the next few weeks, it migrates to the base of the neck. During migration, the thyroid remains connected to the tongue by a narrow canal, the thyroglossal duct. Follicles of the thyroid begin to make colloid in the 11th week and thyroxine by the 18th week. This section does not cite any references or sources. (January 2008) Please improve this section by adding citations to reliable sources. Unverifiable material may be challenged and removed. At the microscopic level, there are three primary features of the thyroid: FeatureDescriptionFolliclesThe thyroid is composed of spherical follicles that selectively absorb iodine (as iodide ions, I-) from the blood for production of thyroid hormones. Twenty-five percent of all the body's iodide ions are in the thyroid gland. Inside the follicles, colloids rich in a protein called thyroglobulin serve as a reservoir of materials for thyroid hormone production and, to a lesser extent, act as a reservoir for the hormones themselves.Thyroid epithelial cells (or "follicular cells")The follicles are surrounded by a single layer of thyroid epithelial cells, which secrete T3 and T4.Parafollicular cells (or "C cells")Scattered among follicular cells and in spaces between the spherical follicles are another type of thyroid cell, parafollicular cells, which secrete calcitonin. The primary function of the thyroid is production of the hormones thyroxine (T4), triiodothyronine (T3), and calcitonin. Up to 80% of the T4 is converted to T3 by peripheral organs such as the liver, kidney and spleen. T3 is about ten times more active than T4.[5] Thyroxine is synthesised by the follicular cells from free tyrosine and on the tyrosine residues of the protein called thyroglobulin (TG). Iodine is captured with the "iodine trap" by the hydrogen peroxide generated by the enzyme thyroid peroxidase (TPO)[6] and linked to the 3' and 5' sites of the benzene ring of the tyrosine residues on TG, and on free tyrosine. Upon stimulation by the thyroid-stimulating hormone (TSH), the follicular cells reabsorb TG and proteolytically cleave the iodinated tyrosines from TG, forming T4 and T3 (in T3, one iodine is absent compared to T4), and releasing them into the blood. Deiodinase enzymes convert T4 to T3.[7] Thyroid hormone that is secreted from the gland is about 90% T4 and about 10% T3.[5] Cells of the brain are a major target for the thyroid hormones T3 and T4. Thyroid hormones play a particularly crucial role in brain development during pregnancy.[8] A transport protein (OATP1C1) has been identified that seems to be important for T4 transport across the blood brain barrier.[9] A second transport protein (MCT8) is important for T3 transport across brain cell membranes.[9] In the blood, T4 and T3 are partially bound to thyroxine-binding globulin, transthyretin and albumin. Only a very small fraction of the circulating hormone is free (unbound) - T4 0.03% and T3 0.3%. Only the free fraction has hormonal activity. As with the steroid hormones and retinoic acid, thyroid hormones cross the cell membrane and bind to intracellular receptors (α1, α2, β1 and β2), which act alone, in pairs or together with the retinoid X-receptor as transcription factors to modulate DNA transcription[1]. The production of thyroxine and triiodothyronine is regulated by thyroid-stimulating hormone (TSH), released by the anterior pituitary. The thyroid and thyrotropes form a negative feedback loop: TSH production is suppressed when the T4 levels are high, and vice versa. The TSH production itself is modulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus and secreted at an increased rate in situations such as cold (in which an accelerated metabolism would generate more heat). TSH production is blunted by somatostatin (SRIH), rising levels of glucocorticoids and sex hormones (estrogen and testosterone), and excessively high blood iodide concentration. An additional hormone produced by the thyroid contributes to the regulation of blood calcium levels. Parafollicular cells produce calcitonin in response to hypercalcemia. Calcitonin stimulates movement of calcium into bone, in opposition to the effects of parathyroid hormone (PTH). However, calcitonin seems far less essential than PTH, as calcium metabolism remains clinically normal after removal of the thyroid, but not the parathyroids. It may be used diagnostically as a tumor marker for a form of thyroid cancer (medullary thyroid adenocarcinoma), in which high calcitonin levels may be present and elevated levels after surgery may indicate recurrence. It may even be used on biopsy samples from suspicious lesions (e.g. swollen lymph nodes) to establish whether they are metastasis of the original cancer. Calcitonin can be used therapeutically for the treatment of hypercalcemia or osteoporosis. In areas of the world where iodine (essential for the production of thyroxine, which contains four iodine atoms) is lacking in the diet, the thyroid gland can be considerably enlarged, resulting in the swollen necks of endemic goitre. Thyroxine is critical to the regulation of metabolism and growth throughout the animal kingdom. Among amphibians, for example, administering a thyroid-blocking agent such as propylthiouracil (PTU) can prevent tadpoles from metamorphosing into frogs; conversely, administering thyroxine will trigger metamorphosis. In humans, children born with thyroid hormone deficiency will have physical growth and development problems, and brain development can also be severely impaired, in the condition referred to as cretinism. Newborn children in many developed countries are now routinely tested for thyroid hormone deficiency as part of newborn screening by analysis of a drop of blood. Children with thyroid hormone deficiency are treated by supplementation with synthetic thyroxine, which enables them to grow and develop normally. Because of the thyroid's selective uptake and concentration of what is a fairly rare element, it is sensitive to the effects of various radioactive isotopes of iodine produced by nuclear fission. In the event of large accidental releases of such material into the environment, the uptake of radioactive iodine isotopes by the thyroid can, in theory, be blocked by saturating the uptake mechanism with a large surplus of non-radioactive iodine, taken in the form of potassium iodide tablets. While biological researchers making compounds labelled with iodine isotopes do this, in the wider world such preventive measures are usually not stockpiled before an accident, nor are they distributed adequately afterward. One consequence of the Chernobyl disaster was an increase in thyroid cancers in children in the years following the accident. [2] The use of iodised salt is an efficient way to add iodine to the diet. It has eliminated endemic cretinism in most developed countries, and some governments have made the iodination of flour mandatory. Potassium iodide and Sodium iodide are the most active forms of supplemental iodine. [edit] Hyper- and hypofunction (affects about 2% of the population)
Medication linked to thyroid disease includes amiodarone, lithium salts, some types of interferon and IL-2.
Nodules of the thyroid may or may not be cancer. Medical ultrasonography can help determine their nature because some of the characteristics of benign and malignant nodules differ. The main characteristics of a thyroid nodule on high frequency thyroid ultrasound are as follows: Possible cancerBenign characteristicsirregular bordersmooth bordershypoechoic (less echogenic than the surrounding tissue)hyperechoicmicrocalcifications-taller than wide shape on transverse study-significant intranodular blood flow by power Doppler--"comet tail" artifact as sound waves bounce off intranodular colloid Ultrasonography is not always able to separate benign from malignant nodules with complete certainty. In suspicious cases, a tissue sample is often obtained by biopsy for microscopic examination. Thyroid scintigraphy, imaging of the thyroid with the aid of radioactive iodine, usually iodine-123 (123I), is performed in the nuclear medicine department of a hospital or clinic. Radioiodine collects in the thyroid gland before being excreted in the urine. While in the thyroid the radioactive emissions can be detected by a camera, producing a rough image of the shape (a radiodine scan) and tissue activity (a radioiodine uptake) of the thyroid gland. A normal radioiodine scan shows even uptake and activity throughout the gland. Irregularity can reflect an abnormally shaped or abnormally located gland, or it can indicate that a portion of the gland is overactive or underactive, different from the rest. For example, a nodule that is overactive ("hot") to the point of suppressing the activity of the rest of the gland is usually a thyrotoxic adenoma, a surgically curable form of hyperthyroidism that is hardly ever malignant. In contrast, finding that a substantial section of the thyroid is inactive ("cold") may indicate an area of non-functioning tissue such as thyroid cancer. The amount of radioactivity can be counted as an indicator of the metabolic activity of the gland. A normal quantitation of radioiodine uptake demonstrates that about 8 to 35% of the administered dose can be detected in the thyroid 24 hours later. Overactivity or underactivity of the gland as may occur with hypothyroidism or hyperthyroidism is usually reflected in decreased or increased radioiodine uptake. Different patterns may occur with different causes of hypo- or hyperthyroidism. A medical biopsy refers to the obtaining of a tissue sample for examination under the microscope or other testing, usually to distinguish cancer from noncancerous conditions. Thyroid tissue may be obtained for biopsy by fine needle aspiration or by surgery. Needle aspiration has the advantage of being a brief, safe, outpatient procedure that is safer and less expensive than surgery and does not leave a visible scar. Needle biopsies became widely used in the 1980s, but it was recognized that accuracy of identification of cancer was good but not perfect. The accuracy of the diagnosis depends on obtaining tissue from all of the suspicious areas of an abnormal thyroid gland. The reliability of needle aspiration is increased when sampling can be guided by ultrasound, and over the last 15 years, this has become the preferred method for thyroid biopsy in North America. Levothyroxine is a stereoisomer of thyroxine which is degraded much slower and can be administered once daily in patients with hypothyroidism. Graves' disease may be treated with the thioamide drugs propylthiouracil, carbimazole or methimazole, or rarely with Lugol's solution. Hyperthyroidism as well as thyroid tumors may be treated with radioactive iodine. Percutaneous Ethanol Injections, PEI, for therapy of recurrent thyroid cysts, and metastatic thyroid cancer lymph nodes, as an alternative to the usual surgical method. Thyroid surgery is performed for a variety of reasons. A nodule or lobe of the thyroid is sometimes removed for biopsy or for the presence of an autonomously functioning adenoma causing hyperthyroidism. A large majority of the thyroid may be removed, a subtotal thyroidectomy, to treat the hyperthyroidism of Graves' disease, or to remove a goitre that is unsightly or impinges on vital structures. A complete thyroidectomy of the entire thyroid, including associated lymph nodes, is the preferred treatment for thyroid cancer. Removal of the bulk of the thyroid gland usually produces hypothyroidism, unless the person takes thyroid hormone replacement. Consequently, individuals who have undergone a total thyroidectomy are typically placed on thyroid hormone replacement for the remainder of their lives. Higher than normal doses are often administered to prevent recurrence. If the thyroid gland must be removed surgically, care must be taken to avoid damage to adjacent structures, the parathyroid glands and the recurrent laryngeal nerve. Both are susceptible to accidental removal and/or injury during thyroid surgery. The parathyroid glands produce parathyroid hormone (PTH), a hormone needed to maintain adequate amounts of calcium in the blood. Removal results in hypoparathyroidism and a need for supplemental calcium and vitamin D each day. In the event the blood supply to any one of the parathyroid glands is endangered through surgery, the parathyroid gland(s) involved may be re-implanted in surrounding muscle tissue. The recurrent laryngeal nerves provide motor control for all external muscles of the larynx except for the cricothyroid muscle, also runs along the posterior thyroid. Accidental laceration of either of the two or both recurrent laryngeal nerves may cause paralysis of the vocal cords and their associated muscles, changing the voice quality. Large goiters that cause symptoms, but do not harbor cancer, after evaluation, and biopsy of suspicious nodules can be treated by an alternative therapy with radioiodine. The iodine uptake can be high in countries with iodine deficiency, but low in iodine sufficient countries. The 1999 release of rhTSH thyrogen in the USA, can boost the uptakes to 50-60% allowing the therapy with iodine 131. The gland shrinks by 50-60%, but can cause hypothyroidism, and rarely pain syndrome cause by radiation thyroiditis that is short lived and treated by steroids. There are several findings that evidence a great interest for thyroid disorders just in the Medieval Medical School of Salerno (XII Century). Rogerius Salernitanus, the Salernitan surgeon and author of "Post mundi fabricam" (around 1180) was considered at that time the surgical text par excellence all over Europe. In the chapter "De bocio" of his magnus opum he describes several pharmacological and surgical cures, some of which nowadays are reappraised quite scientifically effective.[10] In modern times, the thyroid was first identified by the anatomist Thomas Wharton (whose name is also eponymised in Wharton's duct of the submandibular gland) in 1656.[11] Thyroid hormone (or thyroxin) was identified only in the 19th century.  Position of the Thyroid in Males and Females  Section of the neck at about the level of the sixth cervical vertebra. Muscles of the neck. Anterior view. The arch of the aorta, and its branches. Superficial dissection of the right side of the neck, showing the carotid and subclavian arteries. Diagram showing common arrangement of thyroid veins. Sagittal section of nose mouth, pharynx, and larynx. Muscles of the pharynx, viewed from behind, together with the associated vessels and nerves. The position and relation of the esophagus in the cervical region and in the posterior mediastinum. Seen from behind. Section of thyroid gland of sheep. X 160. The thymus of a full-term fetus, exposed in situ.  Thyoid histology هذا بحث منقول من موقع بيكيديا على هذا الرابط http://en.wikipedia.org/wiki/Thyroid | |||
| |  |
| | رقم المشاركة : [3] | ||
 | يعطيك العافية اخوي الرعد بصراحة مب عارفة شلون اشكر | ||
| |  |
| | رقم المشاركة : [4] | ||
 | Thyroid cancer Causes [IMG]http://*********************.revolutionhealth.com/*********************images/images-image_popup-thyroid.jpg[/IMG] Your thyroid gland is composed of two lobes that resemble the wings of a butterfly separated by a thin section of tissue called the isthmus. The thyroid takes up iodine from the food you eat and uses it to manufacture two main hormones, thyroxine (T-4) and triiodothyronine (T-3). These hormones maintain the rate at which your body uses fats and carbohydrates, help control your body temperature, influence your heart rate and regulate the production of protein. Your thyroid gland also produces calcitonin, a hormone that regulates the amount of calcium in your blood. The thyroid contains two main types of cells. Follicle cells make the thyroid protein thyroglobulin and produce and store thyroxine and triiodothyronine. Other cells, called C cells (parafollicular cells), produce calcitonin. The distinction is important because each type can give rise to different types of cancer. Papillary and follicular cancers develop in follicle cells. They account for the great majority of thyroid cancers, can usually be completely removed with surgery and generally result in an excellent prognosis. Medullary cancer, on the other hand, arises in the thyroid's C cells and is generally more aggressive and harder to treat than papillary and follicular cancers are. The types of thyroid cancer include:
This is the most common type of thyroid cancer. It develops from thyroid follicle cells and usually appears as a single mass in one lobe of the thyroid. Anyone, including children, can develop papillary cancer, but it's most common in women who are between 30 and 50 years of age. Although most papillary cancers grow slowly, they often spread to the lymph nodes early in the course of the disease. This usually doesn't affect the outlook for recovery, which is generally excellent when the cancer is small and its spread limited to the lymph nodes in your neck. The prognosis isn't as positive for people with very large tumors or in the rare cases when papillary cancer has invaded tissues other than the lymph nodes. But even papillary tumors that have spread to the lungs or bone often can be successfully treated with radioactive iodine (radioiodine). Follicular cancer (follicular carcinoma, follicular adenocarcinoma) This type of cancer is more aggressive and affects a slightly older population than does papillary cancer. Follicular tumors don't usually spread to the lymph nodes but are likely to invade the veins and arteries within the thyroid. From there, they may spread to organs such as your lungs and bone. Medullary cancer (medullary carcinoma) Rather than arising from follicle cells, this type of thyroid cancer develops in calcitonin-producing C cells. These tumors usually make calcitonin along with carcinoembryonic antigen (CEA) - a protein produced by certain cancers. Both are released into the bloodstream and can be detected by blood tests. But in many cases, medullary cancer may spread to the lymph nodes or other organs before a lump is detected or blood tests show an increase in calcitonin or CEA. There are three main types of medullary cancer:
This rare form of thyroid cancer is sometimes called undifferentiated cancer because it looks very different from normal thyroid tissue under a microscope. It appears to develop from an existing, undiagnosed papillary or follicular cancer. Anaplastic cancer is extremely aggressive, spreads rapidly to the lymph nodes and trachea, and then to other organs, especially the lungs and bone. For that reason, it's often not curable surgically by the time it's diagnosed. Unfortunately, other therapies, such as radiation, aren't usually successful in controlling anaplastic cancer. Thyroid lymphoma This rare type of cancer doesn't develop from thyroid follicular cells or C cells. Instead, it starts in immune system cells called lymphocytes. Although most lymphomas begin in the lymph nodes, some occasionally appear in other organs, such as the thyroid. What causes thyroid cancer? Healthy cells grow and divide in an orderly way. This process is controlled by DNA - the genetic material that contains the instructions for every chemical process in your body. When DNA is damaged or altered, changes occur in these instructions. One result is that cells may begin to grow out of control and eventually form a tumor - a mass of malignant cells. In the case of thyroid cancer, DNA damage can occur from exposure to environmental contaminants such as radiation, from the aging process or, in medullary cancers, from genetic causes:
| ||
| |  |
| | رقم المشاركة : [5] | ||
 |  | ||
| |  |
| | رقم المشاركة : [6] | |||
 | وهذي صوره للغده وفيها المسميات باللغه الانجليزيه ان شاء الله تفيدك http://www.fpnotebook.com/ThyroidAnterior.gif | |||
| |  |
| | رقم المشاركة : [7] | |||
 | غلا عمري ان شاء الله الاعضاء ماقصرو معاك | |||
| |  |
| | رقم المشاركة : [8] | |||
 | الجميع ماقصرو ونتمنى ان تتواجدي معنا باستمرار | |||
| |  |
 |
| مواقع النشر (المفضلة) |
| |